Some Obstetrical History: Dying to Have a Baby - The History of Childbirth
Dr. Ian Carr
Professor Emeritus, Faculty of Medicine, University of Manitoba
Two great curses haunted natural childbirth from ancient times, the shrunken pelvis and obstructed labour. With urbanization and hospitalization, puerperal fever became common. Because so often mothers died in childbirth and children in infancy, attitudes towards birth and babies were different from ours. Parents expected that children would die in infancy, and death in childbirth was an expected tragedy.
In developed countries, child mortality is now low, and maternal mortality a rare catastrophe; the natural phenomena of birth up till this century can be best understood by a quotation from an eighteenth-century Scottish obstetrician, William Smellie:
Case 454 Natural delivery; death from cold afterwards. In the beginning of my practice I was sent for in a cold frosty night to a poor woman in the country, who had been safely delivered. As she was excessively cold all the time of labour from the badness of the house, the want of clothes and the necessities of life, I gave her husband some money to go to an alehouse at a mile distance and bring from thence something comfortable. I left directions with the midwife to get her warm as soon as possible. The fellow got drunk and did not return for several hours. I was told afterwards that the cold and shivering continued, and the poor creature died the next morning. Indeed as there was little or no fuel for fire, both the midwife and I caught severe colds; for it was a lone house and at a distance from any inhabited neighbourhood.
The classical Romans had considerable obstetric skill. Soranus (A.D. 98-138) wrote a textbook of obstetrics which was used until the sixteenth century. Soranus described podalic version, and the use of the obstetric chair, and gave detailed instructions on the care of the new- born, "boiled water and honey for the child for the first two days, then on to the mother's breast."
These skills largely disappeared during the Dark Ages; there is little record of obstetric practice after this until early modern times. Presumably obstetrics during the Dark Ages was a matter for the mid-wife, and no doubt, free of the possibilities of infection found in a large hospital, she did a good job. We know some of the superstitions: women were whipped to induce labour. There is a tale of a mediaeval German Empress in whose labour room twenty men were whipped, two to death. She went into successful labour. We know of Dr Wertt of Hamburg in 1522, who had the effrontery to dress up in woman's clothes to gain entry to a labour room; and who was thereafter burned at the stake. The new medical knowledge of the Renaissance was spread by the printing press. The first book on obstetrics in English --The Birth of Mankynde was produced in 1544 by Thomas Raynalde. In it he considers such problems as caesarean section. The whole process of pregnancy was considered by Jacob Rueff (1500-1558) in his De conceptu generationis hominis, published in 1554. There followed a spate of publications applying the new techniques of anatomy and anatomical illustration to obstetrics.
Ambrose Pare (1509-1589) apprenticed in a small rural town, and then further trained in the famous Paris Hotel Dieu in the midst of a busy surgical life, had like most surgeons of his time obstetric skills. Of podalic version he wrote:
...he must lift him [the baby] up gently, and so turn him that his feet come first--then little by little turn the whole body from the womb.
Pare induced labour by dilating the cervix, and first used nipple shields, made of lead, to protect cracked nipples. William Harvey who discovered the circulation of the blood practised obstetrics, and wrote a major text on Reproduction, giving for instance the first description of involution of the uterus, post partum.
Obstructed labour terrified women --William Smellie wrote:
Case 386. A neglected transverse lie. The arm had been pulled down by the midwife till the shoulder was at the vulva. Twenty four hours later Smellie was sent for, cut off the swollen arm, performed internal version and brought down one leg. This came off on pulling, so the other leg was brought down and the same thing happened again. Ultimately delivery was accomplished with the crotchet. The woman behaved with great courage.
Obstetric Forceps
Obstetric forceps, a major innovation in the treatment of obstructed labour were introduced by the Chamberlen family about 1650, and were kept as a family secret for many years. William Chamberlen and his family were Huguenots who emigrated to England in 1569. In the year of Chamberlen's death, physicians at Marburg realised that St. Anthony's Fire, an epidemic disease characterised by severe limb pains, was caused by eating spoiled rye contaminated by the fungus now known as ergot. Pregnant women very often aborted. The midwives of the district gave several grains of ergot to induce labour
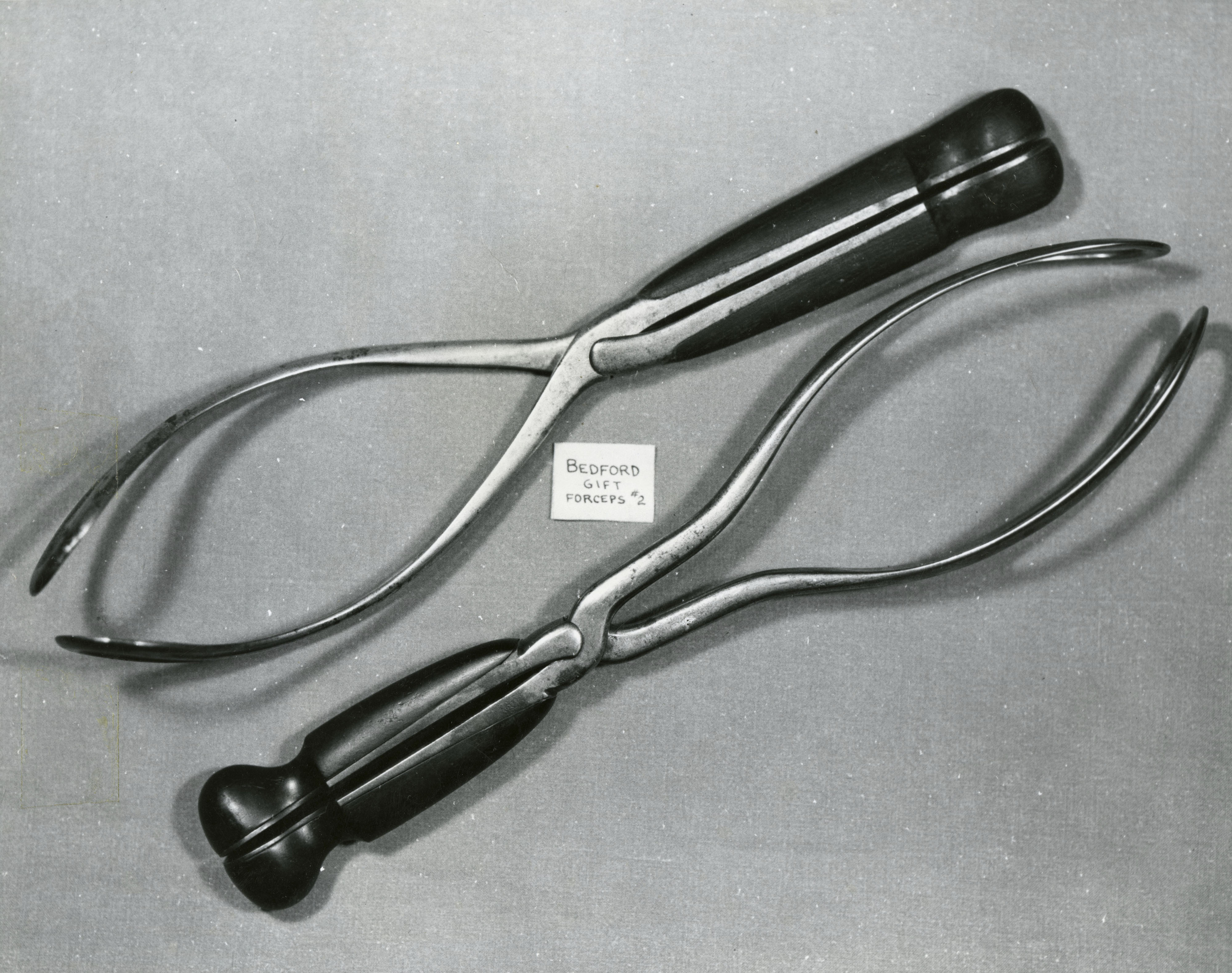
The eldest and the youngest of William Chamberlen's children--Peter I and Peter II, both became physicians, and one of them (probably Peter I) invented a crude but effective form of obstetric forceps. They took the machine with them to a confinement, in an ornate carved gilded box, so heavy that it took two men to carry it. They kept their secret, to the annoyance of the public, and their fellow physicians.
Peter III died in 1683, and his widow hid a box in an attic of their house, containing three sets of obstetric instruments, including forceps in various stages of development, and a fourth pair of forceps, at an experimental stage.
Around 1700, Hugh offered to sell the forceps to Mauriceau, the famous French obstetrician, without success; but the secret gradually leaked, though we do not know quite how. By 1733, Chapman's midwifery text contained a description of forceps, and their use, and in European urban centres they were widely used.
The real pioneer in the use of obstetric forceps was William Smellie (1697-1763). Smellie practised family medicine in Lanark, Scotland for a number of years. He carried in his pocket, wherever he went his three tried remedies, spirits of hartshorn, tincture of castor, and liquid laudanum. An account rendered to one of his patients still exists: "Seven pounds sterling for amputation and cure of your leg."
As a young doctor, he was particularly interested in obstetrics, and distressed by the sadness of the results. He started to use such forceps as were then available, with little success. He set off in 1739, to study in London, and briefly Paris. Finally he returned to London, and set up in a very mean apothecary's shop, on or just off Pall Mall, with a paper lantern at the door --Midwifery taught for five shillings.
Midwifery was still beset by prudery and practised under the bed-clothes. But students came, and he offered free care to indigent women, thus providing clinical teaching material. It was a flourishing school at the right time. The first obstetric wards in Britain opened in Jermyn St. in 1739, to become in 1752 the General Lying In Hospital, in 1791, Queen Charlotte's Hospital. Smellie's lectures were published to be followed by his Treatise on Theory and Practice of Midwifery 1752.
Smellie's great achievement was the proper use of forceps. His forceps were either wood or steel padded with leather and a the simple ("English") lock. They were short, and he advocated their use only after the head had entered the pelvis. He controlled their use by a scientific study of pelvic measurements, introducing the diagonal conjugate measurement, measured by the fingers from the arch of the pubis, to the sacrum.
He realised that most of those who had been rickety in their infancy ...are commonly narrow and distorted in the pelvis, and consequently subject to tedious and difficult labours. He was the first to realise that the foetal head rotated during labour, the first to apply the forceps to the aftercoming head in a breech delivery, and the first to revive an asphyxiated infant by inflating the lungs with a silver catheter.
In several countries, notably Britain there was considerable strife between the mid-wives, and the man-midwives, male physicians who competed with the local wise-woman for the task and the financial reward. It was felt to be undesirable that men should be involved in so intimate a process. One Elizabeth Nihell wrote of Smellie that he was a great horse godmother of a he-midwife and charged that he and others taught midwives wrong, so that they would be called in to help.
Caesarean Section
The other treatment for obstructed labour is Caesarean section. The oldest reference to Caesarean section on the dead mother was in the Roman Law of Numa Pompilius. (715-673 BC). There is no doubt that this was sometimes successful, but there is no good documentation of section with survival of both mother and child.
The practice was revived at the Renaissance, and good stories abound. One tells how in 1500 Jacob Nufer, a Swiss sow gelder called in all thirteen of the local midwives unsuccessfully. Then he called in the two local lithotomists, in vain. So he did the obvious and did the job himself. Mother and child survived, she to bear him several more children.
Over the next two centuries a few more sections were probably carried out with survival of mother and child. The most clearly documented acount is that by Scipione Mercurio (1540- 1615) given in his text first published in 1596. He gives a detailed and illustrated account of how to make the incision, with four strong assistants to hold the patient down. Afterwards he applied a decoction of artemisia, agrimony, betony, mallow, flowers of pomegranate, dried roses, birthwort, sedge and sweet smelling bulrushes in sour black wine. The survival statistics were not clear.
There is a gap in the historical record; then in 1793 in Manchester England, Jane Foster, whose pelvis was deformed after being crushed accidentally, survived a Caesarean section by Dr James Barlow; the baby was dead. There followed a period during which several mothers and babies were lost, and in which the opponents of section offered symphysiotomy and the use of the crotchet to destroy the foetus. Section won out, as the better of two bad options.
At this time the famous French obstetrician Baudeloque published a book reviewing the 31 successful Caesarean sections done in the previous fifty years. A copy of the English translation of this book passed to a backwoods Virginia doctor, who recorded the fact that he performed caesarean section on his own wife by annotation in the margin of his own copy "14 Jany 1794 JB on EB up 9 Feby walked 15 Feby Cured on 1 March." The mother survived for 25 years, and the baby for 77. The operation was done under laudanum, on two planks set across two barrels. Dr Jesse Bennett removed both ovaries remarking as he did so that he would not be subjected to such an ordeal again. But Caesarian section was rarely attempted and rarely successful before Listerian antisepsis. Thus in 1849, Dr Radford of Manchester reported that he had lost 3 mothers and babies out of 5 attempts, even with anaesthesia; in 1900, Dr Sinclair at the same centre reported 10 out of 10 successes.
Anaesthesia
Women until 150 years ago bore children without anaesthesia; there was nothing better than poppy mandragora and henbane. Most women feared the pains of child-birth greatly. When J.Y.Simpson introduced ether anaesthesia, followed by chloroform, there were cries from the pulpit that God was being deprived of the deep earnest cries of women in labour. Those who trumpeted forth in sorrow shalt thou bring forth children were by and large male. Simpson quoted back to them: And the Lord caused a deep sleep to fall upon Adam; and he slept; and he took one of his ribs, and closed up the flesh instead thereof. Simpson described the first midwifery case in which he used chloroform thus:
I placed her under the influence of chloroform, by moistening, with half a tea spoonful of the liquid, a pocket handkerchief, rolled up into a funnel shape, and with the broad or open end of the funnel placed over her mouth and nostrils .........after the delivery she observed that she had enjoyed a very comfortable sleep,...but would now be more ready for the work before her. ...it was a matter of no small difficulty to convince the astonished mother that the labour was over and that the child presented to her was really her "own living baby."
Puerperal Fever
Puerperal fever is as old as medicine. Hippocrates described how Thasus wife of Philonus died after twenty days. Paul Malouin described it at the Hotel Dieu in 1746:
The disease usually commenced with a diarrhoea; the uterus became dry, hard and painful....pain in the bowels....pain in the head and sometimes cough. On opening the bodies, curdled milk was found on the surface of the intestines, a milky serous fluid in the hypogastrium....the stomach, the intestines and the uterus when carefully examined, appear to have beeen inflamed.
Mortality in Paris, Vienna and other European centres rose in such epidemic years as 1772 to 20% of all delivered mothers. Alexander Gordon (1752-1799) of Aberdeen Scotland was the first to identify the cause of puerperal fever.
I will not venture positively to assert that the Puerperal Fever and Erysipelas are precisely of the same specific nature... (but) that they are concomitant epidemics I have unquestionable proofs. For these two epidemics began in Aberdeen at the same time, and afterwards kept pace together; they arrived at their acme together, and they both ceased at the same time. After delivery the infectious matter is readily and copiously admitted by the numerous patulous orifices, which are open to imbibe it, by the separation of the placenta from the uterus."
Gordon sectioned three cases and found pelvic peritonitis.
After Gordon other cases were reported which tied puerperal fever to one specific physician; the final proofs came from Holmes and Semmelweiss.
Oliver Wendell Holmes was not an obstetrician, but Professor of Anatomy & Physiology at Harvard, and an elegant essayist. His attention was drawn to a case where a physician performed an autopsy on a patient with puerperal fever, and then attended several women who developed puerperal fever. He, himself, died of septicaemia, soon thereafter.
In his famous essay on Puerperal Fever published in 1842 Holmes emphasized that a physician attending a midwifery case should not take an active part in an autopsy on a patient dead of puerperal fever, erysipelas, or even peritonitis. He noted that "if one case of puerperal fever arises in a physician's practice there is an increased risk of a second, two cases suggest that the physician should do no obstetrics for at least a month, and three prima facie evidence that he is the source of the contagion. The time has come when the existence of a private pestilence in the sphere of a single physician should be looked upon not as a misfortune, but as a crime."
Controversy was extensive, but change began to occur. The conclusive evidence was provided by Ignaz Philip Semmelweiss (1818-1862) who qualified in Vienna in 1844, and became assistant at the Vienna Lying In Hospital soon after. At that time unmarried Viennese mothers were admitted at the sixth or seventh month of pregnancy, and discharged to the Foundling Hospital. Survivors became wards of the state, the males in due course cannon fodder for the Emperor's army.
Semmelweiss with the backing of the great morbid anatomist Rokitansky began to do autopsies on women with puerperal fever and noted that a high death rate from this disease was found only in First Clinic wards attended by students, and not in Second Clinic wards attended by midwives. Women begged to go to the latter. There were various suggestions as to cause--overcrowding, unwed maternity, but Semmelweiss showed that these were more common in Second Clinic. When his colleague Kolletschka died of a dissecting wound, Semmelweiss saw the parallel, and came to the right conclusion. He instructed his students to scrub their hands in chloride of lime before having any contact with the patient. The death-rate fell: 1846--11.4%; 1847--3.8%; 1848--1.27% cf 1.33% in Second Clinic.
Semmelweiss wrote:
Puerperal fever is caused by conveyance to the pregnant woman of putrid particles derived from living organisms, through the agency of the examining fingers....... Consequently must I make my confession that God only knows the number of women whom I have consigned prematurely to the grave.
There was still controversy, but wherever the doctrine was accepted the incidence and mortality of puerperal fever fell dramatically. Semmelweiss died tragically; he was a manic depressive, and was on August 1 1865 admitted to a lunatic asylum, where a minor cut on his right hand was noted, contracted during a gynaecological operation. He died of septicaemia.
In 1879, Pasteur and his colleagues demonstrated that the cause of puerperal fever was usually streptococcus.
