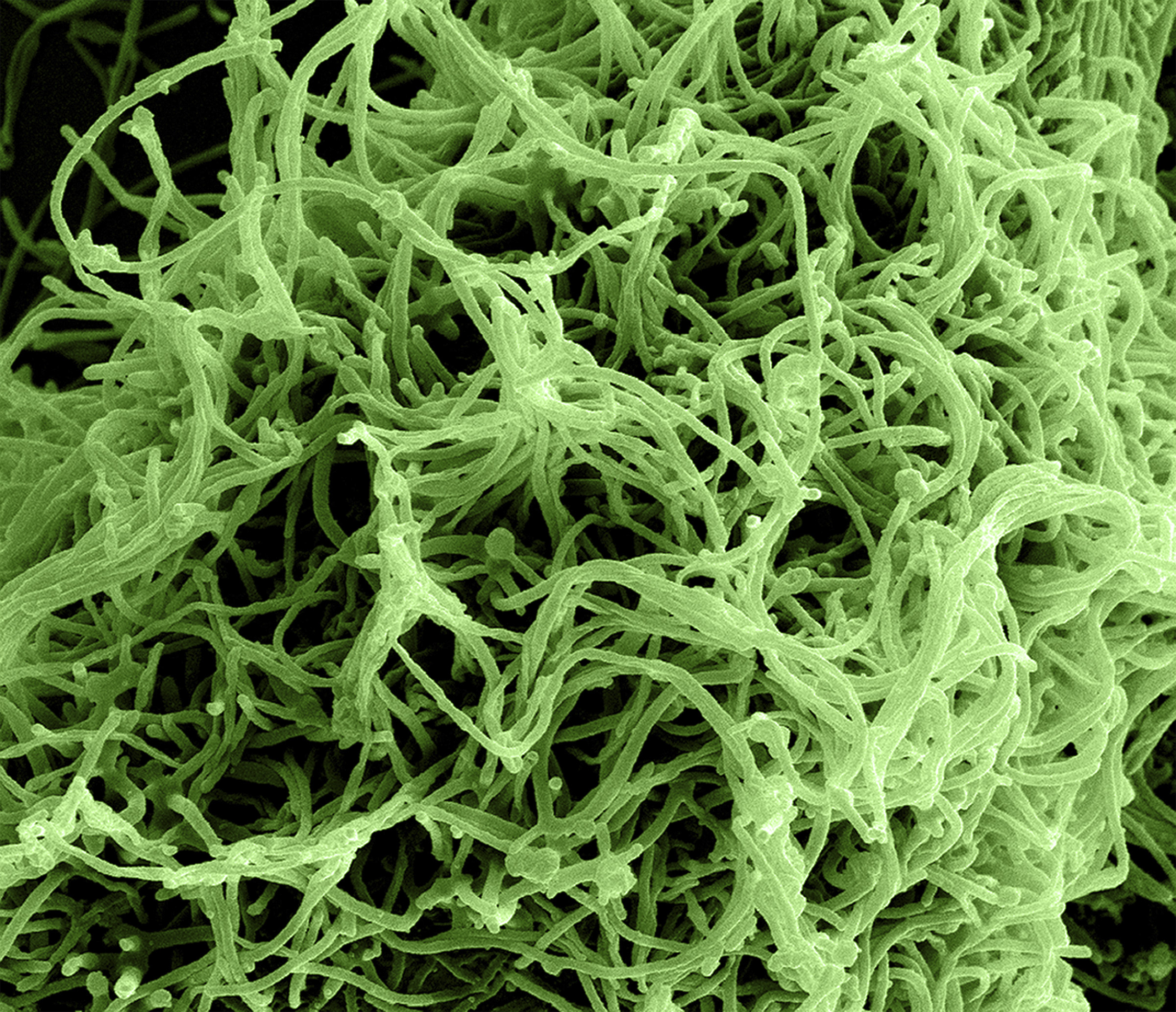
"Produced by the National Institute of Allergy and Infectious Diseases (NIAID), under a magnification of 25,000X, this digitally-colorized scanning electron micrograph (SEM) depicts numerous filamentous Ebola virus particles budding from a chronically-infected VERO E6 cell."
ID# 17770. National Institute of Allergy and Infectious Diseases (NIAID), 2014. Available at http://phil.cdc.gov/phil/
A Short History of Infectious Diseases
Infectious diseases thrive on close contact of populations. Throughout history, populations have bunched closer and closer -- nomadic people became agrarian, and once again shifted as rural became urban. People have much more contact with one another as we move forward, and as a result, much to the chagrin of medical professionals, infectious diseases flourish.
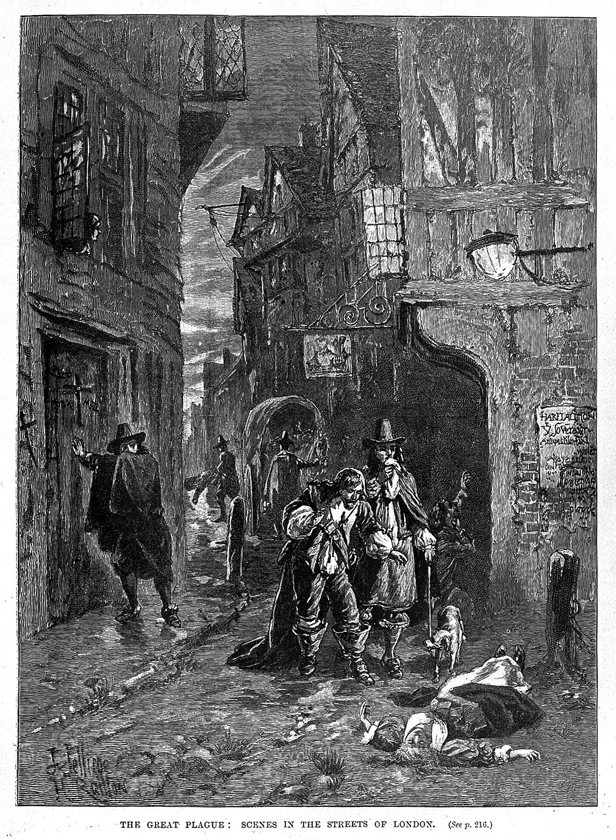
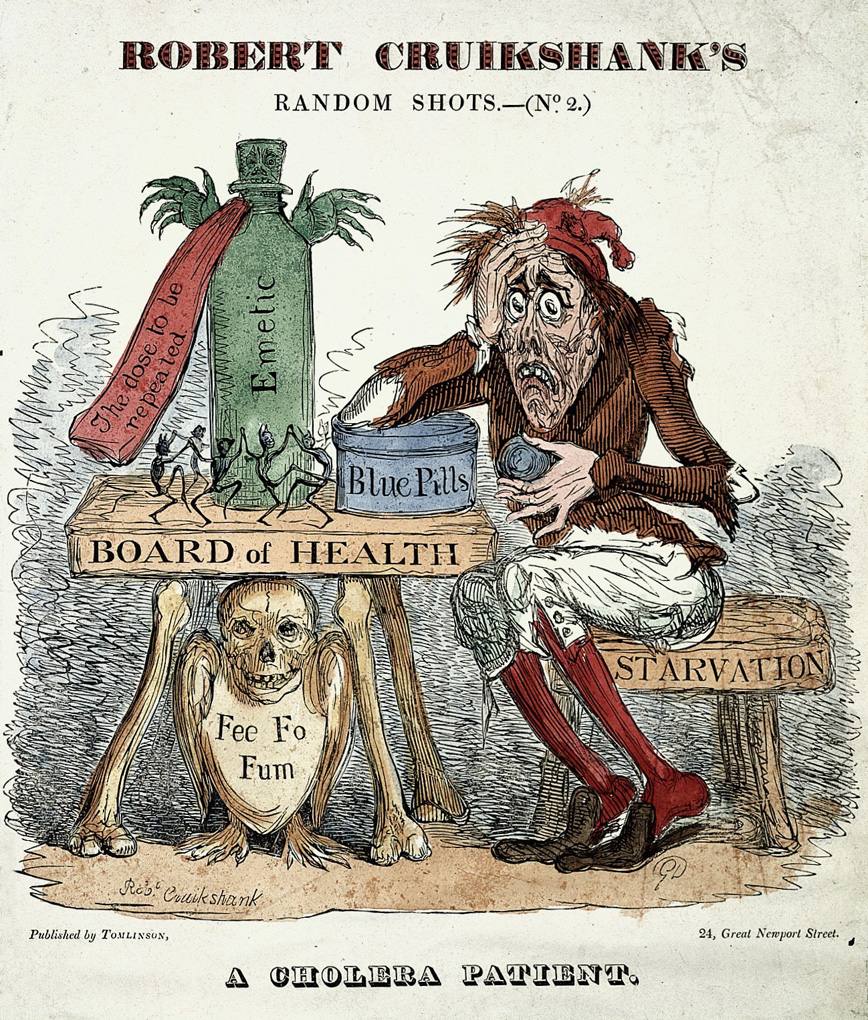
"Two men discovering a dead woman in the street during the Great Plague of London, 1665. Wood engraving by J. Jellicoe after H. Railton." Nineteenth century.
L0001879. Wellcome Library, London, England. Work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/
The bubonic plague is believed to be the disease responsible for the Black Death, a mid-fourteenth century epidemic in Western Europe that killed between one quarter to one third of Europe’s population.1 The Black Death was disastrous, as Jacalyn Duffin describes, "people abandoned their urban homes to wander in the country; sick family members were left to die. Corpses were shunned, and officials tried to establish controls and forced criminals to heap bodies into mass graves."2 Symptoms of the plague are flu-like, including fever and headaches, along with inflamed lymph nodes. Mortality rates are extremely high (around 40 to 60 percent) in untreated cases. Plague epidemics reemerged in Italy (1630 and 1656), England (1665), and Southern France (1720). While the cause of the plague is now known to infect humans when bitten by fleas hosting the bacterium Yersinia pestis, the plague left a trail of human carnage in its wake.3
Another early infectious disease epidemic was syphilis. The first recorded incidence of syphilis was in Naples in the mid-1490’s.4 Though its origins are unknown, scholars have theorized that the disease was brought from the New World to the Old.5 The symptoms of syphilis include skin lesions, bone degeneration, paralysis, blindness, and death (most often due to infections from skin lesions). Unfortunately, syphilis continues to elude medical researchers and a cure does not currently exist. As such, the disease has not been eliminated or even controlled.6
Germ theory, the theory that certain diseases are caused by microscopic organisms, was first proposed by Girolamo Fracastoro in the mid-sixteenth century. Fracastoro posited that diseases are caused by the spread of "seeds." Yet, it was not until the late seventeenth century that Anton van Leeuwenhoek came up a microscope that was powerful enough to view unicellular organisms.7
With germ theory, sanitation became important to reduce the threat of infection. Sir Joseph Lister, in the late nineteenth century, was an early proponent of antiseptic procedures, especially in the operating room where Lister spent most of his time.8 To this day, sanitation is paramount in the medical profession.
From the nineteenth and into the twentieth century, three factors greatly reduced the incidence of infectious diseases: sanitation, hygiene, and public health education. Due to the widespread acceptance of germ theory in the mid to late nineteenth century, sanitation was taken much more seriously. Indoor plumbing and urban sewer systems became more commonplace. These developments were important to try to reduce infectious diseases, as urbanization picked up speed and populations amassed in cities.
In the twentieth century, the advent of antibiotics kept infectious diseases at bay. In 1928, Alexander Fleming discovered penicillin and transformed the fight against infectious diseases. Essentially a mould that kills harmful bacteria, penicillin curbed and eliminated many infectious diseases such as tuberculosis. Yet, while this "magic bullet" continues to save lives, antibiotic-resistant diseases persist and are becoming more common.9
Despite much progress in the knowledge of microorganisms, we are still vulnerable to a multitude of diseases. SARS, Ebola, and the Avian Flu are just some of the recent infectious diseases that affect the world. While a permanent solution to infectious disease has not been found, medical professionals will continue to search for closure.
Infectious Diseases in Manitoba
Infectious diseases have long been part of Manitoban history. Carr and Beamish recount some of the early epidemics in the Red River Colony: smallpox in 1781-82 and 1801-02; measles and whooping cough in 1819-20 and 1827-28; whooping cough in 1834; and influenza in 1835-37.10 In 1846, a measles epidemic prevented colonists from seeding their fields.11
Smallpox was among the worst offender, killing many. Michael B.A. Oldstone claims over 300 million people worldwide died from smallpox in the twentieth century.12 Smallpox causes a severe skin rash containing pus-filled blisters all over the body. Smallpox is extremely contagious and can be transmitted through the air or through contact of the pustules.13 Though smallpox is theorized to have infected humans as early as 10,000 BC, the oldest convincing evidence of smallpox was found on the remains of Ramses V, an Egyptian pharaoh who died in 1157 BC. Smallpox pits were found on his mummified remains.14 In the sixteenth century, European settlers brought the disease to North America, where Native Peoples lacked natural immunity to this debilitating and foul disease. 15
In hopes of developing an immunity to smallpox, people attempted to contract a mild version of the disease through contact with the pustules, a technique known as variolation. While variolation has a very high success rate, it is still a dangerous method of gaining immunity to smallpox, as well as being difficult to find an appropriate source of the disease.
In the late eighteenth century, Edward Jenner observed cowmaids in the English countryside did not have visible scarring on their faces, scarring being a telltale sign of having had smallpox. Jenner deduced the cowmaids gained immunity from smallpox by being in contact with cowpox, closely related to a mild form of smallpox. After testing his hypothesis, in 1798 he published An inquiry into the Causes and Effects of the Variolae Vaccinae, his discoveries of successfully administering the first vaccine.16
Beginning in 1967, the World Health Organization began a campaign to eradicate smallpox.17 Fortunately for us and future generations, smallpox has been successfully eradicated worldwide.
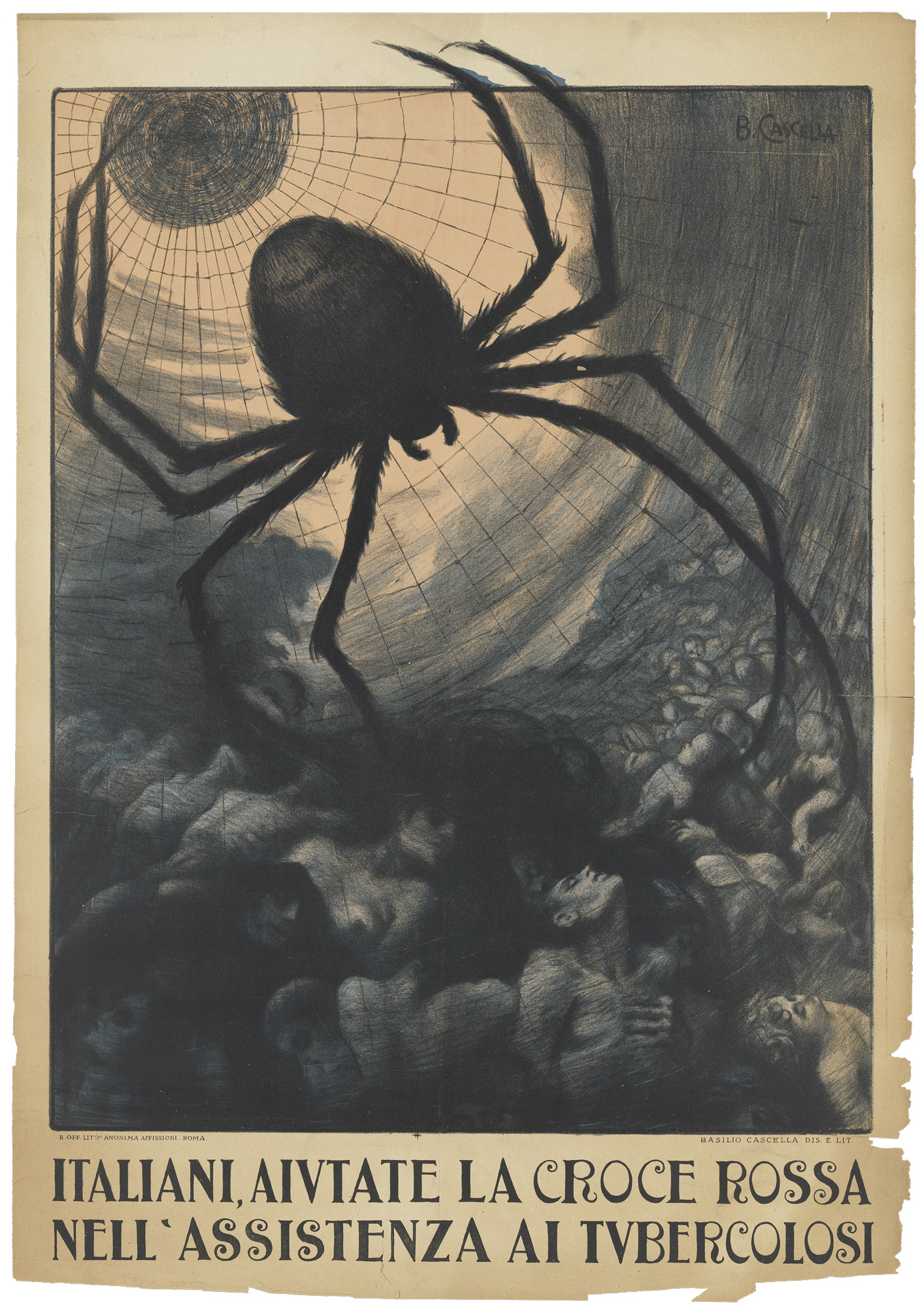
"Lithograph poster appealing for help to care for sufferers of tuberculosis, which is depicted as a spider. Basilio Cascella for the Italian Red Cross, c. 1920."
L0077050. Wellcome Library, London, England. Work available under Creative Commons Attribution only licence CC BY 4.0 http://creativecommons.org/licenses/by/4.0/
Tuberculosis was and continues to be a debilitating infectious disease. TB affects the Aboriginal population disproportionately. This is due to a variety of factors. One factor that Health Canada cites is diabetes and HIV/AIDS being more common among First Nations. Because of these higher incidences, the patient's immune system will be weaker, resulting in the patient being more susceptible to tuberculosis.18 For more information regarding tuberculosis and First Nations in Canada, please see Health Canada's report, "Summary of Epidemiology of Tuberculosis in First Nations Living On-Reserve in Canada, 2000-2008."
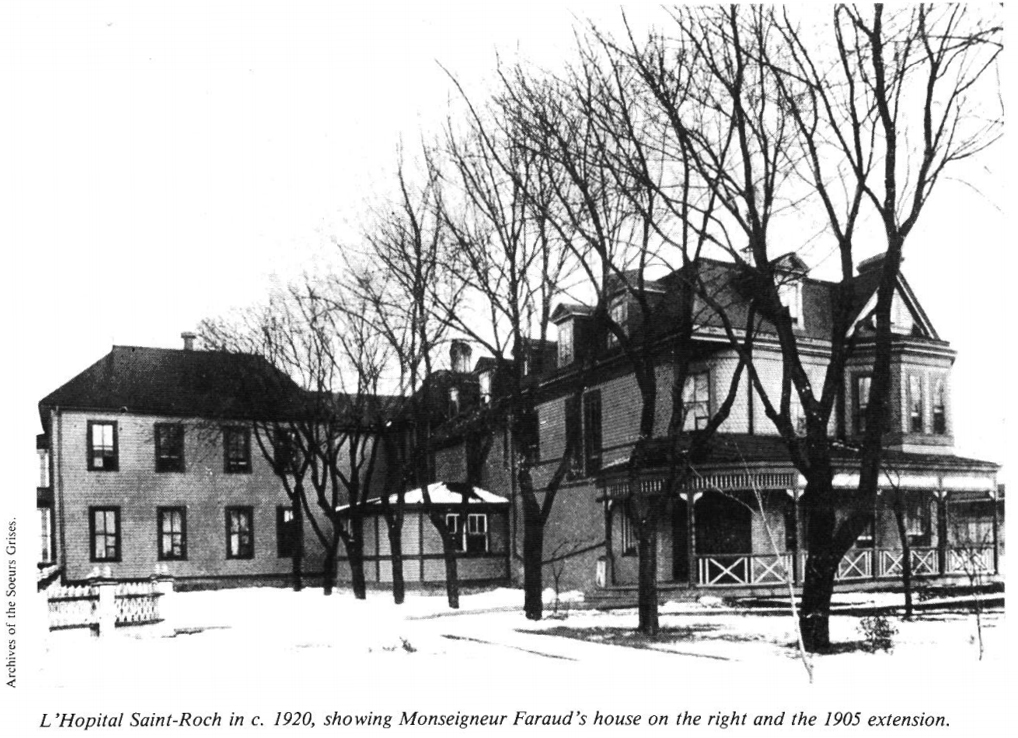
ASGM L052_Y1_C
St. Roch Hospital, St-Boniface, Facade, 1921
In Year past: report of the City of Winnipeg Historical Buildings Committee. Winnipeg: Historical Building Committee, 1979-. Arch/FA FC 3396.7 W56 Note: 1984
Used with permission from the Archives of the Soeurs Grises
Two of Winnipeg's hospitals specializing in infectious diseases were St. Roch's Hospital and King George Hospital. Located at 351 Tache Avenue in the City of St. Boniface (now a neighbourhood in Winnipeg), St. Roch's Hospital opened in November of 1895 in response to tuberculosis and infectious fevers not adequately served by the St. Boniface General Hospital.19 Hospital staff required an area of isolation for infectious patients that the St. Roch Hospital now provided. The hospital was closed to infectious patients in 1942, as patients were adequately served at the St. Boniface General Hospital. The building was demolished in 1984.20
King George's Hospital, close to south-central Winnipeg, opened in 1914 to deal with cases of typhoid fever, scarlet fever, and smallpox. Later, the majority of Winnipeg's polio patients were sent to King George. Due to declining rates of infectious diseases, especially polio, the isolation ward was closed in 1967 and the building was later demolished in 1999 to make way for the Riverview Health Centre.21
HIV/AIDS
Human Immunodeficiency Virus (HIV) is a virus which affects a patient's immune system and results in chronic illness. This leaves the patient susceptible to a multitude of infections and other serious health complications. As the patient's immune system becomes weaker and weaker, their body can no longer fight off infections. At this stage, the disease is known as Acquired Immunodeficiency Syndrome (AIDS).22
HIV is transmitted in one of four ways:
1. Unprotected sexual intercourse
2. Shared needles or equipment for injecting drugs
3. Unsterilized needles (i.e. for tattooing or piercing)
4. During pregnancy, delivery, or breastfeeding (from a HIV positive mother to her child).23
Unlike other infectious diseases such as Ebola or smallpox, once someone is infected with HIV, there is a long period without symptoms. As Barrett and Armelagos write, "the time from initial infection to serious illness is typically more than a decade, during which time the infected host carries high titers of the virus with no detectable symptoms."24 As such, it is paramount to educate people of the seriousness of HIV infection.
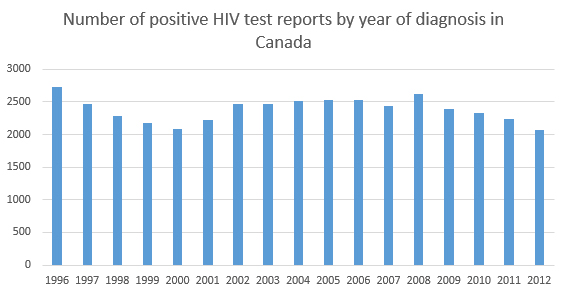
In mid-1981, medical professionals published reports of a new disease, which came to be known as AIDS.25 Globally, HIV/AIDS peaked in the 1990s, although certain parts of Asia, Europe, and Africa still see increased rates.26Africa remains the most significant area affected by HIV/AIDS. Though rates are declining, HIV/AIDS is still a significant disease, one that should not be forgotten about. In 2006, Helene D. Gayle claims nearly 30 million people are infected with HIV.27 As HIV/AIDS prevention is proven to produce lower rates of the disease, education on HIV/AIDS prevention is the key to eliminate this disease once and for all.
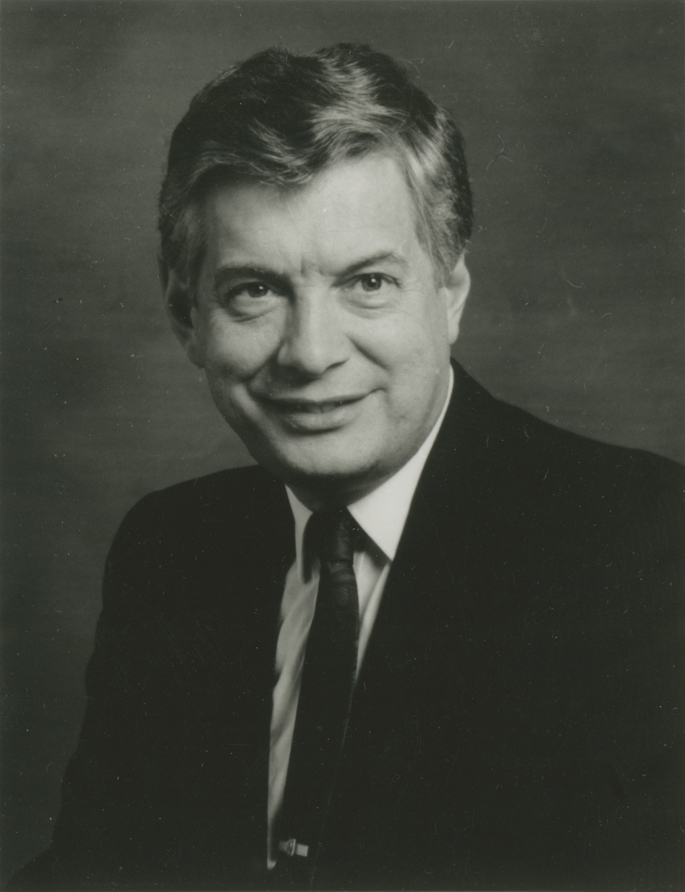
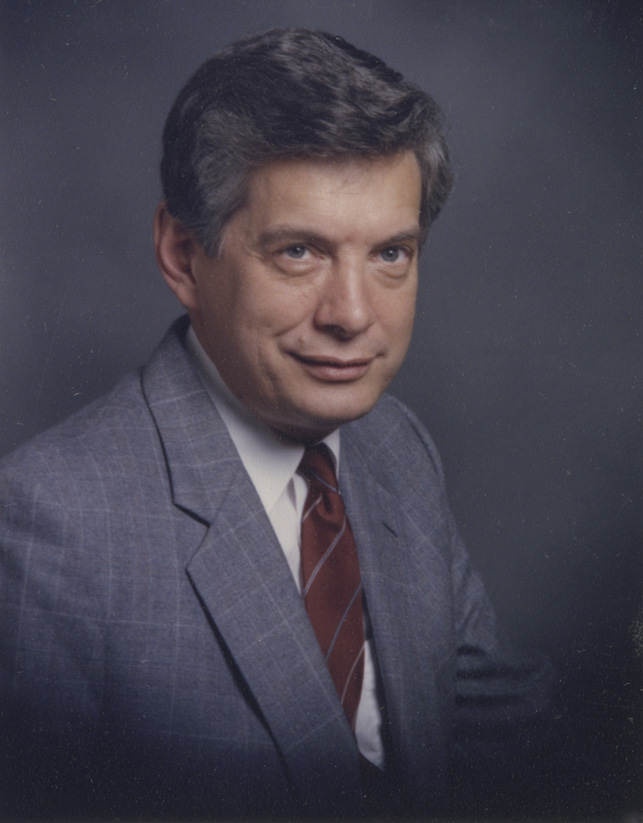
MPC.1.0.196C
University of Manitoba College of Medicine Archives
Dr. Allan Ronald
Allan Ronald has devoted his life to furthering HIV/AIDS research, along with making the University of Manitoba "Canada's premier site for infectious disease."28
Born in Portage La Prairie, Manitoba, Ronald graduated from the University of Manitoba's medical school in 1961.
In 1971, he founded the Infectious Diseases program at the University of Manitoba, considered one of Canada's foremost post-graduate programs to study infectious diseases. In 1978, he was made the head of the Department of Microbiology.29
In 1980, Ronald was part of a team, that also included Frank Plummer, that established a relationship between the U of M and the University of Nairobi to prevent and care for people affected by sexually transmitted infections. The program is officially called The University of Manitoba/University of Nairobi World Health Organization Research and Training Program in Sexually Transmitted Diseases. This program made numerous major discoveries, including uncovering that breastfeeding contributes to transmitting HIV/AIDS, male circumcision reducing HIV infection in men, and the significance of the immune system in preventing HIV infection among certain individuals.30
Ronald was a part of the initiative to make Winnipeg the home of Canada's National Microbiology Laboratory. He is also a senior scientific advisor for the International Centre for Infectious Diseases.
His many honours and awards include becoming an officer of the Order of Canada (1994), a fellow of the Royal Society of Canada (2001), and the Canadian Medical Association's Starr Award (2003). In 2011, he was inducted into Canada's Medical Hall of Fame.
Though he retired in 2000, he continues to work with the HIV/AIDS Care and Prevention Program in Uganda. He is Distinguished Professor Emeritus at the University of Manitoba in Internal Medicine and Microbiology.
Dr. Allan Ronald speaking on infectious diseases, Winnipeg Free Press, June 8, 2003Somewhere along there, it became obvious that this was not a static field and that there would be new problems and challenges. There's almost never been a year since that there hasn't been, somewhere in the world, the emergence of a new pathogen
Infectious Diseases at the University of Manitoba
The story of infectious diseases at the University of Manitoba begins in 1896, when Gordon Bell was made the first professor of Bacteriology and Pathology.31 In 1904, the University established a chair of Bacteriology and Pathology and made Bell the head.32 In 1911, the field of histology was also added to the department. Bell held this position until 1915, when Pathology and Histology became a new department under the direction of William Boyd. Bell was made head of the newly named Bacteriology and Hygiene.33 In 1919, the department once again changed names to Bacteriology and Serology.

Infectious Diseases building, ca. 1960
MPC4.1.0181, University of Manitoba College of Medicine Archives
After Bell tragically died in 1923, Fred Todd Cadham was made head of the department, as well as succeeding Bell as Provincial Bacteriologist. In 1933, the department was now known as Bacteriology and Immunology.34 When F.T. Cadham retired in 1952, John C. Wilt was made department head shortly after. Under Wilt, the department once again changed names to Medical Microbiology, as immunology was a facet of many different departments. The Department of Immunology became an official department in 1968, under the direction of A. Sehon.35
Allan Ronald was made department head in 1976, when Wilt became the Director of Provincial Diagnostic Services.36 Ronald held this position until 1985, when he became head of Internal Medicine at the U of M. While in this position, Ronald brought to Internal Medicine the clinical sub-specialty of Infectious Diseases, strengthening the teaching and research in the subject.
Working in the department are more than 80 people, including basic scientists, physician scientists, physicians-in-training, graduate students, and support and technical staff. The core disciplines used by the department scientists and trainees in research programs include molecular pathogenesis of microbial disease, immunobiology of infection, molecular mechanisms of antimicrobial action, microbial resistance and epidemiology. Opportunities for training and research collaborations are welcomed by departmental scientists.
The department of Medical Microbiology and Infectious Diseases also has close affiliations with the Health Sciences Centre's and St. Boniface Hospital's Clinical Microbiology departments as well as the National Virology Laboratory and Cadham Provincial Laboratories.
Infectious Diseases Research in Winnipeg

MPC4.1.021D, University of Manitoba College of Medicine Archives
A photograph of the University of Manitoba Faculty of Medicine Cadham Provincial Laboratory in 1980. This building is on William Ave., across the street from the Basic Medical Sciences building.
The Cadham Provincial Laboratory has a long standing relationship with the University of Manitoba. The Cadham Provincial Laboratory is an organization of the Government of Manitoba that is “responsible for several province-wide public health, reference, and diagnostic services”.37 Originally called the “Bacteriological Branch of the Board of Health,” Gordon Bell helped establish the provincial lab in 1897. Ian Carr claims “the province was cleaned up” through the initiatives of Bell.39 At this time, the lab was located at the corner of Kate and McDermot Street beside the newly created Manitoba Medical College. At the time, Bell was also teaching pathology and bacteriology, as head of the Department of Pathology at the U of M. The coordination of teaching between the two institutions has been carried over from the lab’s beginning.38
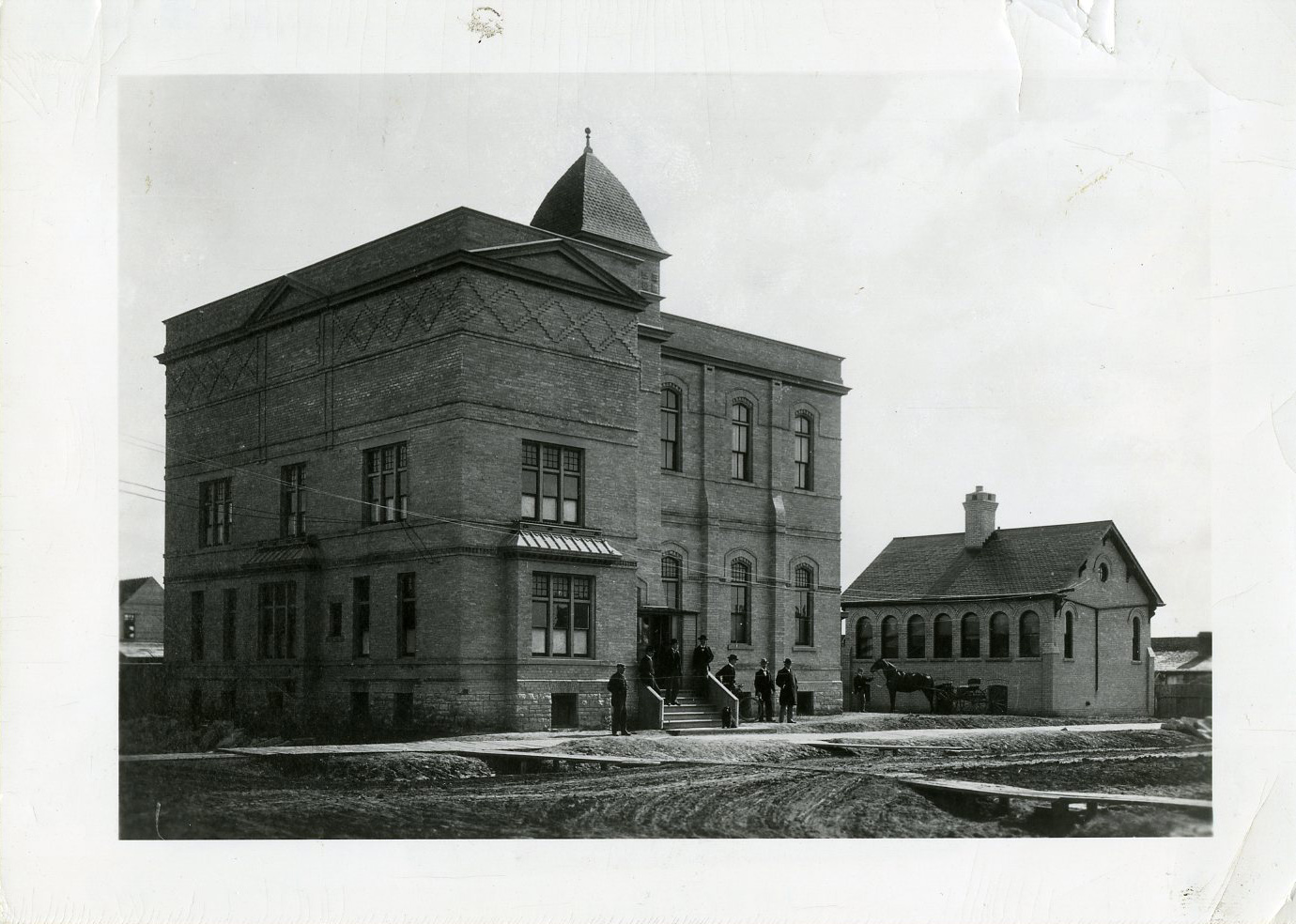
MPC4.1.2, University of Manitoba College of Medicine Archives
Manitoba Medical College, late 1890s.
The original provincial laboratory can be seen beside the larger building of the Manitoba Medical College, at the corner of Kate and McDermot St.
In 1906, the Cadham Provincial Lab moved to 750 Bannatyne Ave., closer to the Winnipeg General Hospital. After Bell died in 1923, Fred T. Cadham took over as Provincial Bacteriologist, the position in charge of the lab. Cadham quickly went to work and transformed the facility into a “centre of diagnostic bacteriology and serology.” He was responsible for instituting vaccinations for diphtheria and allergy studies. Carr once again lavishes praise upon the lab, claiming that because of Cadham and his innovations, the lab "was one of the most influential parts of the medical school”.40

MPC4.1.021A, University of Manitoba College of Medicine Archives
Sketch of Cadham Provincial Laboratory.
When Cadham retired in 1947, the lab’s name changed to “Fred T. Cadham Public Health Laboratory” to honour the former leader. The name was shortened to “Cadham Provincial Laboratory” in 1980.41 After J.C. Wilt left the University of Manitoba, he was the director of the lab from 1976 to 1984. A laboratory in Winnipeg was also named after Wilt. The “J.C. Wilt Infectious Diseases Research Centre,” part of the National Microbiology Laboratory, was recently opened and offers additional space for the national lab’s activities.
The Cadham Provincial Laboratory is currently run by Nicolette Coffin.
In Winnipeg, the National Microbiology Laboratory (NML) stands at the forefront of infectious diseases research. Former Public Health Minister Carolyn Bennett claimed “there’s no question that the National Microbiology Lab is pivotal in our public health-care system in Canada."42
Plans for the NML were initiated in 1987 by Jake Epp, a former Federal Health Minister.43 As discussions took place for where the laboratory would be located, Allan Ronald played a significant role in Winnipeg being chosen. Winnipeg is also conveniently located at the centre of Canada, allowing researchers to fly in and fly out to disease hot spots more quickly.44 When the Laboratory opened in 1999, Frank Plummer was the Scientific Director, a position he held for fourteen years. Matthew Gilmour succeeded Plummer.
The Laboratory conducts research on the world’s deadliest infectious diseases, including Ebola and Lassa fever. Scientists from the NML went to Angola in 2004 and 2005 to fight Marburg hemorrhagic fever, a deadly virus that can cause severe hemorrhaging and organ failure. With their experience in Angola, a vaccine was developed to prevent Marburg.45
International Centre for Infectious Diseases
The International Centre for Infectious Diseases (ICID) is a collaborative research organization that works with scientists and institutions, including the University of Manitoba, to address the problem of infectious diseases.46 Nicholas Hirst, former Winnipeg Free Press editor-in-chief, claims “The International Centre for Infectious Diseases is hugely important for the country.”47 ICID opened in 2004 in Winnipeg, Manitoba. Terry Duguid was the founding president and CEO, from 2004 to 2009. One of the Centre’s first initiatives was to provide high-level training for health professionals and scientists, led by Frank Plummer.48 In November 2009, ICID played host to the International Symposium on Natural Immunity to HIV. ICID’s CEO is currently Heather Medwick.
ICID continues to advance infectious diseases research by working with various institutions and individuals.
References
1. Duffin, Jacalyn. History of Medicine : A Scandalously Short Introduction. Toronto: University of Toronto Press, 2010. 166.
2. Duffin, 165.
3. Duffin, 165-167.
4. Duffin, 168.
5. Barrett, Ron and George J. Armelagos. An Unnatural History of Emerging Infections. Oxford: Oxford University Press, 2013. 45-46.
6. Duffin, 172.
7. Duffin, 170.
8. Duffin, 263.
9. Duffin, 113.
10. Carr, Ian and Robert E. Beamish. Manitoba Medicine: A Brief History. Winnipeg, University of Manitoba Press, 1999. 20.
11. Ibid.
12. Michael B.A. Oldstone. Viruses, Plagues, and History: Past, Present, and Future. Oxford: Oxford University Press, 2010. 53.
13. Oldstone, 56.
14. Oldstone, 56-57.
15. Duffin, 177.
16. Oldstone, 77-79.
17. Oldstone, 94.
18. Health Canada. "First Nations and Inuit Health." Government of Canada. Accessed November 23, 2015. Available at http://www.hc-sc.gc.ca/fniah-spnia/diseases-maladies/tuberculos/index-eng.php
19. Grover, Sheila C. 351 Rue Tache: L'Hopital Saint-Roch. March 1983. 3.
20. Year past: report of the City of Winnipeg Historical Buildings Committee. City of Winnipeg Historical Building Committee. Winnipeg: Historical Building Committee, 1979-. Arch/FA FC 3396.7 W56 Note: 1984.
21. Winnipeg Municipal Hospitals. Winnipeg Municipal Hospital: Redevelopment Program, n.d. 5. Print.
22. Public Health Agency of Canada. "HIV and AIDS." Government of Canada. Accessed November 10, 2015. Available at http://www.phac-aspc.gc.ca/aids-sida/info/index-eng.php
23. Public Health Agency of Canada. "HIV and AIDS." Government of Canada. Accessed November 10, 2015. Available at http://www.phac-aspc.gc.ca/aids-sida/info/index-eng.php
24. Barrett and Armelagos, 89.
25. Helene D. Gayle. "HIV Prevention." In Global HIV/AIDS Medicine, ed. Paul A. Volberding, et. al. 91.
27. Gayle, 91.
28. Mitchell, Catherine. “The Guiding Force.” Winnipeg Free Press. January 30, 2010, H6.
29. Mitchell, Catherine. "A life of chasing bacteria." Winnipeg Free Press. July 23, 1995.
30. "Manitoba MD honoured for work in Africa." Winnipeg Free Press. October 15, 2010.
31. Wilt, John C. “The History of Medical Microbiology at the University of Manitoba.” Manitoba Medical Review. 1970. 16.
32. Stark, Egon. “The History of Medical Bacteriology in Manitoba.” Canadian Journal of Public Health. V. 39 (May 1948). 168.
33. Wilt, 16.
34. Stark, 169.
35. Wilt, 17.
36. Wilt, John C. “Medical Microbiology: An Historical Update, 1970 to the Present, 1987.” Manitoba Medical Review. V.57, no.4. 1987, 141.
37. Wilt, John C. Cadham Provincial Laboratory. Guide to Services. Government of Manitoba. Winnipeg: Cadham Provincial Laboratory, 2012, 4.
38. Carr, Ian and Robert E. Beamish. Manitoba Medicine: A Brief History. Winnipeg, MB: University of Manitoba Press, 1999, 62.
39. Carr and Beamish, 63.
40. Carr and Beamish, 105.
41. Manitoba Health. “Cadham Provincial Laboratory.” Government of Manitoba. Accessed on December 10, 2015. Available at http://www.gov.mb.ca/health/publichealth/cpl/history.html
42. Fallding, Helen. “City lab wows new public health boss: work on SARS garners praise.” Winnipeg Free Press, January 25, 2004.
43. Rabson, Mia and Dan Lett. “A super-lab to fight superbugs: projects in works to expand city’s disease research centre.” Winnipeg Free Press, February 6, 2010.
44. Fallding, Helen. “Manning the Barricades: Arlington Street fortress is at the centre of the battle against SARS, West Nile and mad cow disease.” Winnipeg Free Press, June 8, 2003.
45. Edgar, Patti. “Experts from Winnipeg’s National Microbiology Laboratory are solving mysteries, saving lives and making headlines around the world.” Winnipeg Free Press, March 26, 2006.
46. “Manitoba Movers: Ken Beeson.” Winnipeg Free Press. December 12, 2005. B6.
47. Hirst, Nicholas. “Don’t let the ‘hits’ keep happening.” Winnipeg Free Press. January 28, 2010. A10.
48. “High-level training set in infectious diseases.” Winnipeg Free Press. October 28, 2004. B2.
Banner Images
All work available under Creative Commons Attribution only license CC BY 4.0 http://creativecommons.org/licenses/by/4.0/
1. "The port of Marseille during the plague of 1720. Etching by J. Rigaud after M. Serre. Engraving. Circa 1720." L0007448. London, England: Wellcome Library.
2. Plan of Red River Settlement. Hudson's Bay Company Archives, E.6/13, fo. 1.
3. "Two enlarged images of T-cells one infected with HIV by the Frederick Cancer Research and Development Center. Colour lithograph by Nancy Burson and Kunio Nagashima, National Cancer Institute (US), 1991." L0052324 . London, England: Wellcome Library.
4. Manitoba Medical College, Biochemistry Wing, ca. 1960. A photograph of the biochemistry wing of the Manitoba Medical College/University of Manitoba Faculty of Medicine. This photograph, taken circa 1960, looks northeast from McDermot Ave. UM.MPC.4.1.015A. University of Manitoba College of Medicine Archives.
5. MAN.353A. University of Manitoba College of Medicine Archives.